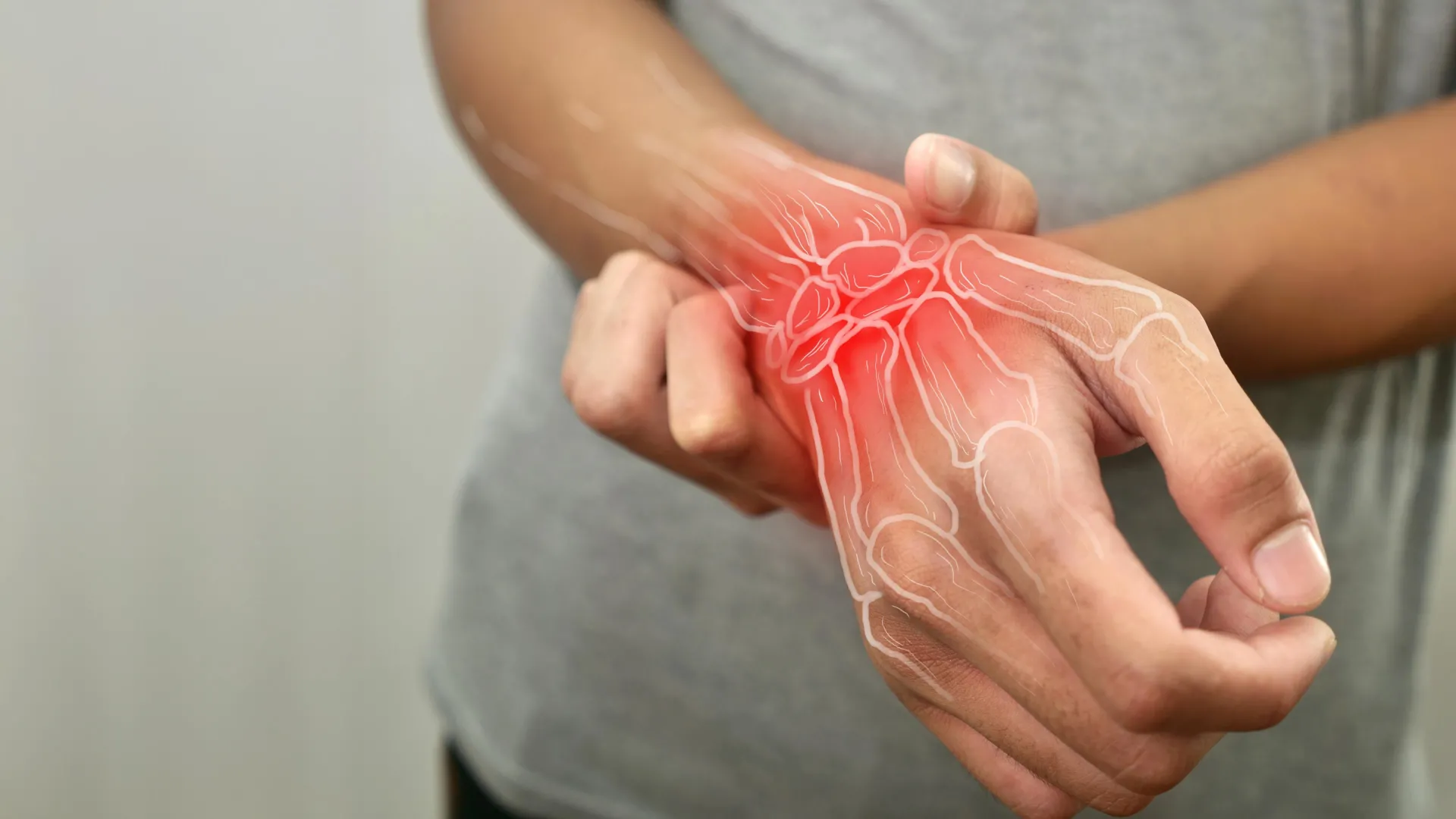
A recent study has revealed that rheumatoid arthritis (RA) begins to develop years before any noticeable symptoms emerge. This groundbreaking research, published on November 26, 2025, highlights how the immune system undergoes significant changes, preparing the body for an autoimmune response long before joint pain or stiffness become apparent.
Conducted by a collaborative team from the Allen Institute, CU Anschutz, University of California San Diego, and the Benaroya Research Institute, the study provides a comprehensive view of the early immune processes associated with RA. The findings, detailed in the journal Science Translational Medicine, indicate that individuals at higher risk for RA show marked immune alterations years prior to the onset of symptoms.
Mapping the Silent Onset of Rheumatoid Arthritis
The researchers monitored participants with ACPA antibodies, known biomarkers for those predisposed to RA, over a span of seven years. Their investigation uncovered several critical factors contributing to the disease’s progression, including widespread inflammation and immune cell dysfunction. This suggests that an autoimmune struggle is already taking place in the body, even in the absence of clinical symptoms.
“Overall, we hope this study raises awareness that rheumatoid arthritis begins much earlier than previously thought,” stated Mark Gillespie, Ph.D., assistant investigator at the Allen Institute and co-senior author of the study. He emphasized the importance of data-driven strategies aimed at disrupting the disease’s development.
The research team discovered that the immune system begins to malfunction and reprogram itself in ways that have not been previously documented. These early changes can offer vital insights for potential preventive measures, as understanding the initial immune response might allow for earlier interventions.
Potential for Early Detection and Intervention
The implications of these findings are significant. The study identifies novel biomarkers and immune signatures that could assist healthcare providers in recognizing which at-risk individuals are most likely to develop RA. Early detection could lead to more vigilant monitoring and timely treatment, potentially halting the disease before it inflicts joint damage.
According to Kevin Deane, M.D./Ph.D., also a co-senior author, the research supports a shift from merely responding to joint damage to proactively preventing RA at its earliest stages. “We expect that going forward, the findings from this study will support additional studies to identify ways to better predict who will get RA,” he said, underscoring the need for targeted biologic interventions.
In summary, the study underscores the importance of recognizing the long-term nature of rheumatoid arthritis and the critical window for intervention that exists before the onset of symptoms. This new understanding may not only enhance current treatment strategies but also pave the way for innovative approaches to prevent the disease altogether, potentially saving patients years of suffering and disability.